What are the three layers of the skin? And what are their roles in scar formation? The skin is a complex organ, and the way it forms scars is part of an intricate and dynamic wound-healing process. The epidermis, dermis, and hypodermis layers of the skin each play pertinent roles in responding to trauma by forming scars. Understanding this is the key to understanding how our bodies heal themselves naturally and ward off infection.
Continue reading to learn more about the three layers of the skin and their roles in scar formation. Read until the end to discover a clinically-proven method for preventing and reducing the appearance of abnormal scars from injuries or surgical procedures.
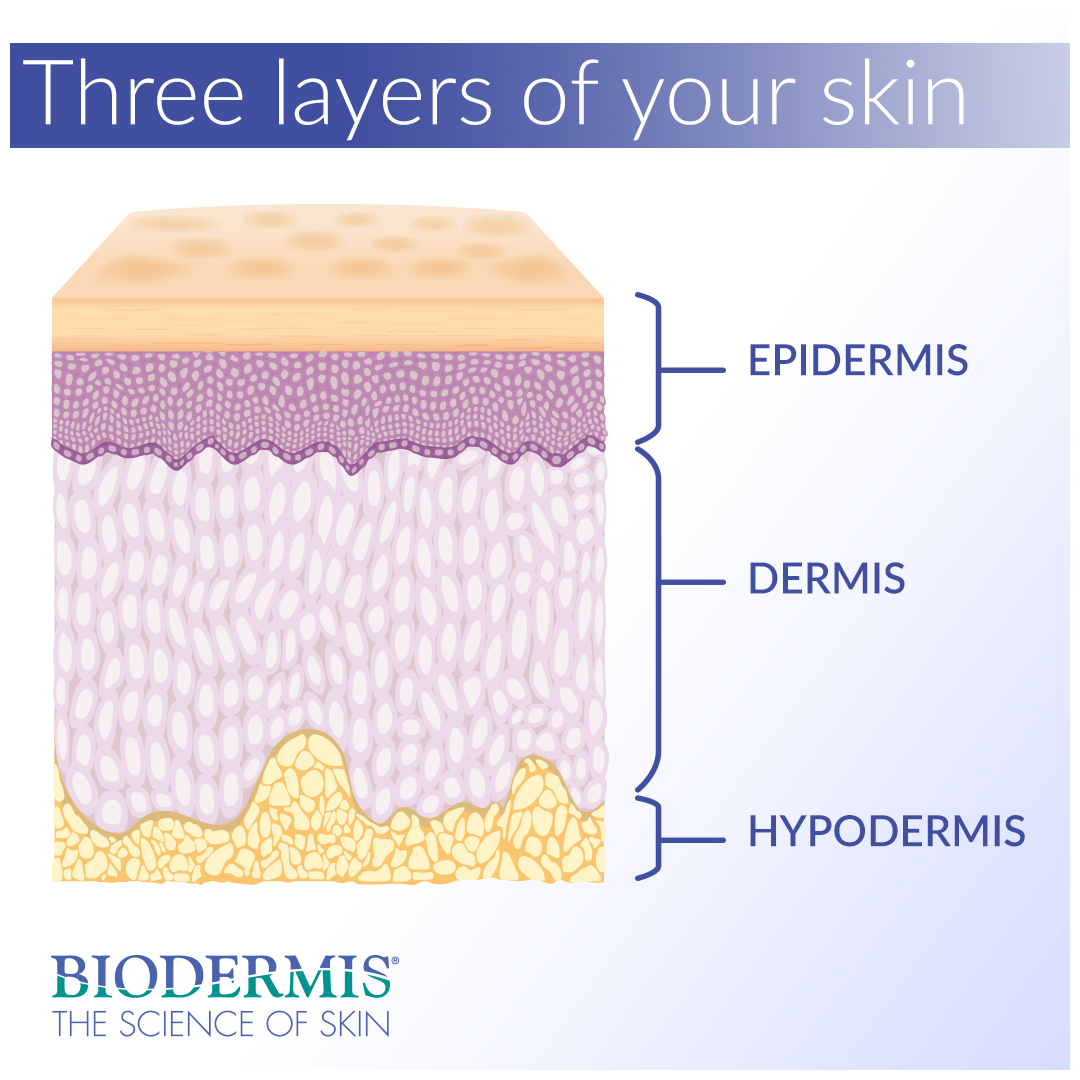
The three layers
The skin is composed of three layers, each of which is vitally important for giving the skin its tone, texture, and ability to heal and produce scars. Scars form in response to burns, infected cuts, acne, injuries and surgical procedures. To understand why our bodies create scars, it’s helpful to first learn about the skin’s three distinct layers.
Epidermis
The epidermis is the top, outermost layer of the skin that acts as a waterproof barrier, protecting the body against environmental pathogens. This layer is also responsible for regulating the amount of water released from the body via sweat glands and other forms of transepidermal water loss. The epidermis is further divided into five sublayers. Under a microscope, the cells of the stratum corneum (top layer of the epidermis) appear flat and scaly.
Dermis
The dermis comprises the thick, vascular layer of the skin lying beneath the epidermis. Tough connective tissues, fibroblasts, and collagen constitute the substance of the dermis. Hair follicles, sweat glands, and mechanoreceptors (touch sensors) are also present in this lively middle layer of the skin. Sweat and other secretions emitted by the dermis reach the skin's surface through small openings called pores.
Hypodermis
The hypodermis, also known as subcutaneous tissue, is the innermost layer of the skin composed mainly of fatty and connective tissue. The hypodermis acts as a padding layer against shock and force trauma. It also works to reserve energy and maintain the body's core internal temperature. Special connective tissue in the hypodermis connects the dermis to muscles and bones in the body.
Scar production and formation
The dermis and epidermis layers of the skin play pertinent roles in scar formation and work to facilitate a natural, biologic process of wound repair. When a person sustains a wound that penetrates the middle layer of the skin—the dermis—the skin repair response begins. Damage to the dermis layer signals fibroblast skin cells to synthesize massive amounts of collagen. The collagen is then sent to the wound site, promoting the growth factor and rebuilding new skin tissue. The epidermis flaunts the new tissue as a scar, which can appear discolored and raised.
Collagen is the predominant structural protein found not only in the skin of human beings but in the bodies of most mammals. The buildup of collagen at the surface of the skin replaces the previous skin tissue with new tissue, resulting in a scar. In some cases, collagen buildup can lead to irregular scar formations that can be unsightly, painful and burdensome.
Types of scars and their appearance
When the skin repairs itself after, say, a tummy tuck, C-section, or breast reduction procedure, we notice its imperfect craftsmanship by the presence of a scar. Scars often appear as irregular skin tissue that differs in complexion and texture from the surrounding skin. More often than not, the cosmetic appearance of scars is the only worry people have after a surgery or accident.
Keloid and hypertrophic scars are cutaneous conditions that sometimes occur as a result of excessive collagen production; these are the scars most people wish to avoid. Keloid scars, also known as keloidal scars, are characterized by lumpy, ropey growths on the skin, often purple or red in color. Keloid scar tissue tends to branch out, covering a larger skin area than the wound itself.
Hypertrophic scars are raised and rigged in appearance, with a red or purple complexion. Though not as severe as keloid scars, hypertrophic scars can still be unappealing and painful. Both of these scar types can occur as a result of a surgical procedure or injury, in addition to any form of piercing or acne scarring.
What can you do to prevent abnormal scarring?
As a first line of defense, one should always seek a topical solution for scar management before resorting to costly surgical procedures or corticosteroid injections. There are many products on the market that claim to reduce scarring, but how do you know which ones are effective? Ingredients like onion extract found in Mederma, and Vitamin E found in other popular scar gels, are pure marketing hype. There are no clinical studies that prove the efficacy of these ingredients in scar therapy, and supporting literature is anecdotal and unreliable.
Topical silicone for scar management has been on the market for over thirty years, and numerous clinical trials support its effectiveness as a prominent scar care solution. Biodermis emerged 30 years ago as the number one provider of medical-grade silicone and offers a variety of unique products. Epi-derm Silicone Gel Sheets by Biodermis come in a multitude of colors, shapes and sizes. And Xeragel is the purest, 100% silicone scar gel currently available.
Biodermis is an innovative market leader with 30 years of expertise in the medical silicone industry. Visit Biodermis.com today to explore a complete range of scar management and post-operative care solutions.
PHYSICIANS AND MEDICAL PROFESSIONALS: REFER OR RESELL?
Biodermis offers custom tailored referral programs designed to simplify and reduce the cost of your patients' post-op care. Additionally, we offer professional pricing if you opt to retail our products. Give us a call at 800.322.3729, and we will be happy to provide additional details on these programs.